Choosing a Mattress to Prevent Pressure Ulcers: Comprehensive Guide
If you’re recovering from the symptoms of a chronic disease and cannot move or change positions without assistance, you may need to take the necessary steps to prevent pressure sores (also known as bed sores, pressure ulcers, or pressure injuries). Health care providers might recommend durable medical equipment to help, so it’s good to know what medical equipment can help and how they can protect you as you recover.
We wrote this comprehensive guide to walk through the best mattresses to prevent pressure sores and other tools you may want to discuss with your doctor or wound care specialist.
Don’t wait to discuss your options—you can reduce your risk of pressure injuries and infections by changing your resting surface, focusing on hygiene, good nutrition, and improving your activity level.
Understanding pressure ulcers
What are pressure ulcers?
The National Pressure Injury Advisory Panel (NPIAP) now uses “pressure injury” as the new clinical term for a pressure ulcer, pressure sore, or bed sore. A pressure injury refers to damaged skin or soft tissue in areas that experience frequent force and friction from sleeping or sitting surfaces.
“The NPIAP changed the terminology years ago from pressure ulcers to pressure injuries because not all are open or ulcerated,” said Leisel Villafania, lead wound care physical therapist at Chapman Global Medical Center in Orange County, California.
Some pressure injuries display a red, irritated patch of skin. Others may display further skin damage, forming an ulcer (or deep pressure injury) that reveals fat, muscle, and sometimes bone. These are classified into four main stages, each requiring a different level of care.
Pressure injury stages simplified
The NPIAP defines four main stages of pressure injuries:
- Stage 1: Skin is intact, but there is red or darkly pigmented skin.
- Stage 2: Soft tissue just under the skin is exposed and may present with blistering.
- Stage 3: The ulcer deepens to expose the fat under the skin.
- Stage 4: The ulcer deepens to expose muscles or bone.
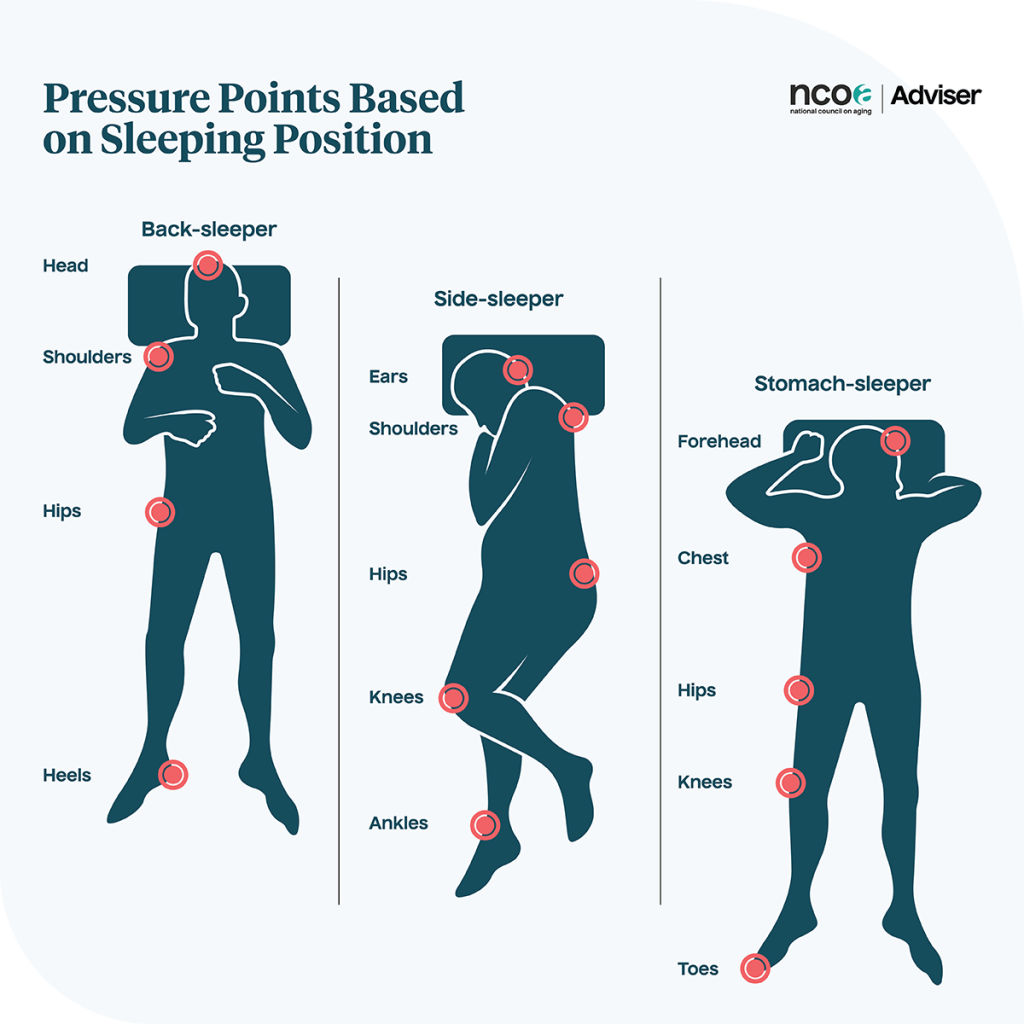
Common areas where pressure ulcers develop
“By definition, pressure injuries occur over areas of the body where a bony prominence is in prolonged contact with an external surface,” said Christopher Norman, geriatric nurse practitioner and primary care provider at the Program of All-Inclusive Care for the Elderly in Central New York (PACE CNY). “For example, if I’m sitting in a recliner chair with my laptop on my lap, my coccyx (tailbone) is in contact with the seat of the chair, and the heels of my feet are in contact with the footrest.”
Depending on the person’s resting position, pressure ulcers often develop around the following areas (according to the National Library of Medicine):
- At the tailbone
- Behind the heel
- On the outside of the hip bone
- Under the ischium (or the pelvic bone we sit on)
The tailbone and heels are the most common location of pressure injuries in older adults, according to research. Villafania, the wound care physical therapist in California, said that some medical devices, like oxygen cannulas, face masks, and Foley catheters, can also cause pressure injuries where they rest or press against the body.
Risk factors for older adults
Pressure injuries often occur in a hospital setting where people are in bed or on a recliner most of the day. But pressure injuries can happen at home, too—according to a study of more than 2,000 older adults who received home care services, 65% developed pressure injuries over time. More than 80% of these people were at severe risk, as identified by an assessment tool called the Braden Scale.
A few factors increase the risk of developing pressure injuries, and some are preventable:
- Sedentary lifestyle: If you stay seated, reclined, or in bed most of the day, you’re at higher risk of a pressure injury. Although some people with mobility issues need caregiving assistance to move about the home, it’s still important to get up often with the right guidance. The more you engage in physical activity, the less likely you’ll develop this injury.
- Restricted activity and mobility: Caregiving assistance is helpful to safely get out of bed and engage in daily activities. Those who cannot change positions easily in bed are more likely to develop pressure, moisture, and friction in certain areas of the body (depending on your preferred resting position). Changing your position can help prevent damaging sensitive skin.
- Moisture buildup: Incontinence or caregiver dependence for toileting can increase the risk of pressure injuries because it encourages moisture buildup in high-risk areas like the tailbone. Changing damp clothes and linens often is important to keep skin healthy. It may also be worth discussing treatment options for bladder and bowel problems, such as seeing a pelvic health physical therapist.
- Sensory deficits: If someone is less able to feel pressure (including painful pressure), they are more likely to develop a pressure injury. This is because they can’t feel discomfort in the area experiencing pressure or friction. Sensory deficits could be a result of conditions that affect how well you feel the things around you. Diabetic neuropathy is one example of a condition that affects your sensation and your ability to heal, which can complicate a pressure injury.
- Poor nutrition: Eating complete and nutritious meals with at least two servings of protein per day can help prevent pressure injuries. Protein is important for healing and strength. Without it, our bodies have a hard time recovering from any wound, injury, or sickness.
- Certain injuries and conditions: Aside from diabetes and incontinence, other chronic diseases that affect our mobility and healing capacity could put you at higher risk for pressure injury. According to geriatric nurse practitioner Norman, this includes blood circulation issues and recent fractures, like a broken leg.
- Aging skin: Norman also mentioned how age-related changes to our skin, like thinning or losing elasticity, can increase the risk of skin injuries.
Importance of prevention
If you or someone you care for identifies with the risks above or has a low-stage bed sore, don’t wait to ask about treatment and management strategies. A pressure injury in its early stage may not seem dangerous, but it’s a warning sign signaling the need for lifestyle changes or adjustments in care.
Once the tissue under the skin is exposed, a pressure injury can lead to infection or restrict daily activities. If you also have a condition like diabetes, it may be more difficult to heal, which can restrict daily activities for a longer period of time.
Key mattress features for pressure ulcer prevention
The best beds to prevent pressure injuries depend on someone’s needs, risk, mobility level, and healing capacity. The following mattress features may help those with pressure injuries:
- Pressure redistribution
- Breathability and temperature regulation
- Solid surface that makes it easy to move
- Durability and easy maintenance
Best mattress types for pressure sore prevention
We asked wound care physical therapist Villafania and geriatric nurse practitioner Norman about the best mattresses to prevent pressure injuries. “Low air loss mattresses and alternating air mattress overlays the most common setups. But, even with these setups, routine monitoring and repositioning are still advised,” said Villafania.
Low air loss mattresses
What they are: Low air loss mattresses have small holes that allow a gradual amount of air to circulate constantly.
How they work: The small holes in these mattresses provide subtle airflow, keeping the skin dry and cool.
Benefits:
- Thick mattress-like design
- Regulates skin temperature and moisture
- Helps people who cannot move or change positions
- Offers some pressure redistribution
Considerations:
- More expensive than other options
- Best suited for a hospital bed
Best for: Those with excessive sweat or incontinence issues who need a long-term solution to offload pressure and promote wound healing

“In my experience, if someone’s wound has a high probability of worsening and they cannot be turned, the low air loss mattress is requested first before the alternating pressure mattress.”
— Leisel Villafania, lead wound care physical therapist at Chapman Global Medical Center in Orange County, California
Air fluidized mattresses
What they are: Air-fluidized mattresses are filled with small ceramic beads that move with airflow.
How they work: Pressurized, warm air moves through a chamber filled with tiny ceramic beads to create a fluid-like feel, which offloads pressure around bony joints prone to pressure injury.
Benefits:
- Helpful for later-stage pressure injuries or other open wounds
- Provides a very low-pressure environment
- Helps manage moisture buildup
Considerations:
- Can feel warmer than other surfaces, so dehydration is a concern, according to research
- The fluid-like surface could make some feel unstable
- Expensive and requires special maintenance
Best for: People with existing severe pressure ulcers or other wounds
Other pressure-relieving mattresses we recommend
If you have a low risk for a pressure injury and just want a pressure-relieving mattress for comfort, you may consider a regular mattress with cushioning and cool materials.
Below, we explain how different types of mattress materials promote comfort (based on our team’s research and testing).
Note: These mattresses are not the best options if you need medical attention to prevent or manage a diagnosed pressure injury.
Adjustable air mattresses
What they are: Adjustable mattresses use air chambers to change firmness level.
How they promote comfort: You can adjust the firmness level of your bed using a remote control to improve comfort.
Benefits:
- Often use foam above air cells for extra cushion
- Allows you to pick your own firmness level that works for your body
- Most queen sizes (or larger) have independent settings for you and a sleeping partner
Considerations:
- More expensive than other types of mattresses
- Does not shift firmness automatically like an alternating pressure mattress
Best for: People who want full control over their mattress’s feel to reduce pressure at painful joints or promote easier movement in bed
Read more about adjustable air mattresses in our Sleep Number alternative review.
Our team recommends the Saatva Solaire as a top adjustable air mattress.
Memory foam mattresses
What they are: These are beds made with foam that conforms to body shape. They may feel soft or dense, although the traditional feel is soft and adaptive.
How they promote comfort: Memory foam distributes body weight evenly and reduces pressure around sharp joints and body curves, like the hip and shoulder.
Benefits:
- Offer contouring and adaptable material
- Often have excellent pressure relief
- Help dampen motion from sleeping partners
Considerations:
- May retain heat. Look for gel-infused designs or phase change materiaⓘ A material that stores or releases heat to maintain a constant temperature built in, which better regulate temperature.
- Memory foam may be more likely to sag and can be difficult to move around on, especially for those with mobility issues
Best for: Those with minimal mobility issues who may sleep with a partner and prefer a “hugged” feeling from their bed
Read more in our best memory foam mattress review.
Our team recommends the Nolah Signature as one of the best memory foam mattresses.
Latex mattresses
What they are: These beds are made with a rubber material naturally derived from trees. They feel similar to foam but are often cooler, more responsive, and more durable.
How they promote comfort: Latex offers pressure relief and contour with more responsiveness and less trapped heat than memory foam.
Benefits:
- Good pressure distribution across the surface
- Naturally cooling and breathable material
- More durable and sag-resistant compared to foam
- Responsive and easy to move on
Considerations:
- Can be expensive and heavy
- May feel too firm for some people
Best for: Older adults with minor mobility issues who want pressure relief without feeling “sucked into” a bed’s material
Read more in our best latex mattress review.
Our team recommends the Nolah Natural as one of the best latex mattresses.
Hybrid mattresses
What they are: Hybrid mattresses combine innerspring coils with layers of foam or latex into one bed.
How they promote comfort: Hybrid mattresses blend the support of coils with the pressure relief of foam.
Benefits:
- Balanced support and pressure relief promote spinal alignment and prevent sagging
- Often provide bounciness and momentum for easier movement without sacrificing cushion
- Airflow through coils can offer better temperature regulation than all-foam options
Considerations:
- Motion transfer between sleeping partners is more noticeable than on foam or latex beds
- Features (like firmness and support) vary
Best for: People who want a balance of support, pressure relief, and mobility-boosting features
Read more in our best hybrid mattress review.
Our team recommends the Helix Midnight Luxe as one of the best hybrid mattresses.
Additional support surfaces
Additional options are available for people who want to reduce pressure buildup. Not all are appropriate for preventing or managing a pressure injury, so make sure you discuss options with your health care provider.
Alternating pressure mattress overlay
What they are: These are mattress pads made with air cells controlled by an air pump to inflate or deflate automatically according to your selected pressure setting. Air cells alternate to reduce pressure buildup in one area of the body.
Benefits:
- Less expensive option compared to low air or air fluidized mattresses
- Often portable due to its pad-like design
- Reduces risk of tissue breakdown
- Pressure intensities can be adjusted
- Durable and versatile
Considerations:
- Sits on top of an existing bed and can shift under the body
- Some users may find the air cells uncomfortable
Best for: People who need a temporary solution and may be at home with a caregiver

Villafania stated that alternating pressure mattress overlays, along with low air loss mattresses, are among the most common setups. Other types of overlays that don’t require power, like gel foam or waffle-patterned mattress overlays, can also help redistribute pressure, depending on your needs.
Pressure relief cushions
What they are: Pressure relief cushions are specialized seat pads that help distribute weight under your buttocks to prevent pressure buildup when sitting on chairs, wheelchairs, or recliners.
Features:
- Can choose from many shapes and sizes
- Come in a variety of materials, including foam or gridded and flexible gel
- Small and easy to adjust
Benefits:
- Offload pressure to prevent force buildup and skin irritation
- Can transfer to different surfaces because of its portable design
- Increase seat height, which makes it easier to stand up
Considerations:
- May need to shop for the right size and shape for your body or seat shape
- Some may shift with movement or position adjustments
- Not all come with washable covers to clean moisture buildup or fluids

People at risk for pressure injuries on the heel may benefit from a similar cushion placed around the foot. These boot-like air-filled cushions hug the foot and heel to protect from pressure buildup when someone is lying down for long periods of time and cannot adjust themselves.
Mattress toppers
What they are: A mattress topper is additional padding placed on top of an existing mattress to change its firmness, support, and pressure relief.
Features:
- Made from various materials, like latex, memory foam, or gel-infused foam
- Can provide additional cushioning for better pressure distribution
- May have cooling properties to help regulate temperature
Benefits:
- Great for those who find their existing mattress uncomfortable
- May help cool down hot sleepers
- A relatively inexpensive option to adjust an existing mattress’s feel
Considerations:
- Does not cycle firmness levels the way alternating pressure mattresses can
- Some may slide around under bed sheets as you move
- Will not compensate for a worn bed with sagging areas that cause pressure
Read more in our best mattress topper review.
Adjustable bed frames
What they are: Adjustable bed frames are remote-controlled and allow body adjustments for more comfortable positioning as you relax or fall asleep.
Features:
- Allow head and foot elevation
- Some models have additional positioning features, like zero-gravity position, neck tilting, lower back support, and the ability to store your favorite positions
- Some advanced models include under-bed lighting to help see pathways at night and prevent falls
Benefits:
- Can redistribute pressure
- Assist movement, like getting in and out of bed
- Claim to aid certain medical issues, like snoring or acid reflux
- Foot elevation can help improve lower body swelling, which impacts skin health
Considerations:
- More expensive than standard bed frames
- Require compatible mattresses
- Not a substitute for a hospital bed that better fits specialized medical equipment for pressure injuries
Read more in our best adjustable beds review.
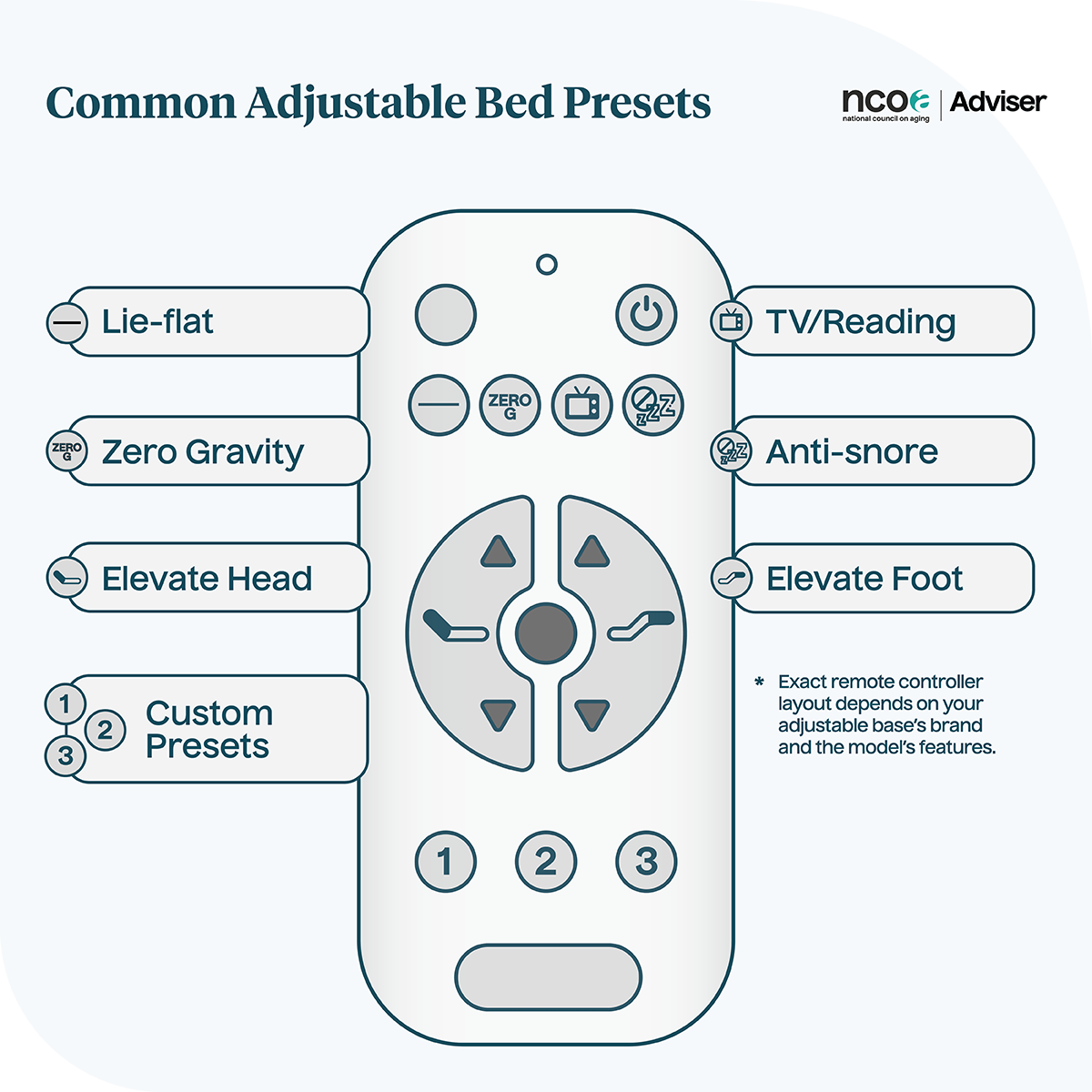

Adjustable beds are not the same as hospital beds. People with caregivers to help manage chronic diseases benefit most from a hospital bed, which has height adjustments, wheels to move the entire bed for patient care, and certain safety features (like rails and a footboard). Hospital beds also pair well with specialized mattresses that use vinyl covers for easy cleaning, which is especially important for those with wounds or incontinence.
Positioning aids
Sometimes, using other types of pillows and sheets can help offload pressure, improve overall comfort, or assist a caregiver when it’s time to change positions. Here are a few positioning aids to consider:
- Wedge pillows: These triangular pillows help elevate your head or legs to help with circulation, swelling, or positioning. Some wedge pillows can also be used under the midsection or hips while side-lying to offload areas at risk of pressure injury.
- Turning sheets: Caregivers may benefit from using a turning sheet (also known as a slide sheet), which helps roll someone into a new position while minimizing friction on areas at risk for pressure injuries.
- Body pillows: Long body pillows aren’t necessarily designed for pressure injuries but can be looped around the body and between or under the legs to help find a comfortable position. These are best for people who want to customize their position in bed for added comfort.
Additional pressure sore prevention strategies
“As the old saying goes, ‘An ounce of prevention is worth a pound of cure,’” said Norman. “Know your risk factors, and ask your health care team how to reduce them.”
Pillows, wedges, and specialized mattresses aren’t the only ways to reduce pressure injury risk. Norman and Villafania often advise the following prevention strategies, but always talk to your health care provider to understand what’s most effective for your body:
- Scheduling exercise, mobility practice with guidance, or position changes
- Eating a balanced diet
- Drinking water to remain hydrated
- Having proper skin care and hygiene, keeping high-risk areas clean and dry
- Checking pressure sites routinely as determined by a health care provider
- Avoiding harsh soaps and irritants on risky areas, especially if a pressure injury already exists
- Watching medical device placement around the body to avoid unnecessary pressure and friction on the skin
Consult a health care professional about pressure ulcers
If you or someone you care for is at risk for a pressure injury, work closely with your health care provider (at home or in a facility) to prevent it. Don’t wait until it begins to damage the skin past the early stages, as this increases the risk of infection. A pressure injury at any stage requires proper monitoring and follow-up care to prevent it from worsening.
Proper equipment, like an air-fluidized bed, can be costly at home. Medicare Part B may help cover some of the cost as long as you have a doctor’s prescription requesting a “pressure-reducing support surface.”
Bottom line
The best mattress to prevent pressure sores depends on your risk, your chronic diseases, and level of care. You may need durable medical equipment designed to offload pressure away from high-risk areas, like an air-fluidized, alternating pressure, or low air loss mattress.
Positioning strategies are not the only way to prevent or manage pressure injuries. Nutrition, hygiene, hydration, and regular movement are also important to keep skin and body healthy.

Frequently asked questions
If you’re concerned about pressure ulcers, it’s important to talk to your doctor to learn how to prevent them. Medical-device mattresses with pressure-relieving features, like air chambers that alter firmness over time, might be the best option. But if your main concern is pressure relief for comfort and sleep quality reasons and you aren’t at risk for pressure injuries, a non-specialized pressure-relieving mattress with cushion and support might be a good choice.
Some mattresses require flipping to prevent sagging and pressure buildup, while others don’t. Check with your mattress brand for the recommended care and maintenance.
Some memory foam mattresses are good at distributing your weight evenly across the surface, which can reduce pressure in certain areas like your hips. But if you’re concerned about developing pressure injuries, talk to your doctor about prevention strategies and consider getting a specialized mattress instead. This may include an alternating pressure mattress or a low air loss mattress.
Have questions about this review? Email us at reviewsteam@ncoa.org.
Sources
- Pressure Ulcers: Learn More — Preventing Pressure Ulcers. National Library of Medicine. Aug. 19, 2022. Found on the internet at https://www.ncbi.nlm.nih.gov/books/NBK326430/
- Edsberg L, et al. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System. Journal of Wound, Ostomy, and Continence Nursing. November 2016. Found on the internet at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5098472/
- Al Aboud, Ahmad and Manna, Biagio. Wound Pressure Injury Management. StatPearls. April 19, 2023. Found on the internet at https://www.ncbi.nlm.nih.gov/books/NBK532897/
- Broderick, Vianna and Cowan, Linda. Pressure Injury Related to Friction and Shearing Forces in Older Adults. Journal of Dermatology and Skin Science. July 12, 2021. Found on the internet at https://www.dermatoljournal.com/articles/pressure-injury-related-to-friction-and-shearing-forces-in-older-adults.html
- Bottega M, et al. The Risk and Prevalence of Pressure Injuries in Older People in the Home Care Service: A Cross-Sectional Study. Journal of Wound Care. Oct. 13, 2023. Found on the internet at https://www.magonlinelibrary.com/doi/full/10.12968/jowc.2023.32.Sup10.ccxi
- Braden Scale (Pressure Ulcer). Shirley Ryan Ability Lab. April 26, 2012. Found on the internet at https://www.sralab.org/rehabilitation-measures/braden-scale-pressure-ulcer
- Fleck C, et al. Use of Alternatives to Air-Fluidized Support Surfaces in the Care of Complex Wounds in Postflap and Postgraft Patients. The Journal of the American College of Certified Wound Specialists. March 21, 2010. Found on the internet at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601929/
- Pressure-Reducing Support Surfaces. Medicare.gov. Found on the internet at https://www.medicare.gov/coverage/pressure-reducing-support-surfaces




