Chronic Conditions and Fall Risk: Cross-Promoting Programs Across the Continuum of Care
7 min read

Related Topics
Have you ever wondered how diabetes and fall risk are connected, or how to engage participants in additional programs? If someone with arthritis is also at risk for a fall, how can we communicate that better to support this person? Promoting evidence-based programs across the continuum of care, or offering a “continuum of programs,” can help participants, program providers, and health care providers to consider these connections and to encourage participation in more than one program to address chronic conditions and fall risk.
What do chronic conditions and fall risk have in common?
Chronic conditions such as arthritis, cardiovascular disease, diabetes, and vision and hearing loss can often lead to developing fall risk factors. Some fall risk factors, such as chronic pain, exercise intolerance, or physical inactivity can be a consequence of a chronic condition and can lead to decreased range of motion, flexibility and strength. Irregular vital signs, visual and hearing loss, and certain medications to treat chronic conditions are also fall risk factors.
According to the NCOA Center for Healthy Aging Falls Database, over 67% of falls prevention program participants indicate that they have multiple chronic conditions, and the top three self-reported are arthritis (66%), heart disease (27%), and diabetes (24%). Sixty-seven percent of participants in falls prevention programs have multiple chronic conditions, which could increase their fall risk.
Evidence-based health promotion programs offer solutions to managing chronic conditions and falls risk by encouraging physical activity, maintaining a healthy weight and a regular sleep schedule. Some programs focus on creating a safe home environment and developing the skills and support to discuss medication management and lifestyle changes with a health care provider.
Why promote a continuum of programming?
While many modifiable risk factors for falls can be addressed through evidence-based programs, for chronic conditions that contribute to increased fall risk, it is important to support and to empower participants to manage their health condition along with support from their health care provider.
For example, a person with arthritis may suffer from painful joints and movement, which may lead to limited activity. When one starts to limit activity due to chronic pain, this can result in limited mobility and muscle weakness. Older adults may also start to limit activity due to a fear of falling. All of these combined, muscle weakness, limited activity, chronic pain, and a fear of falling, can increase fall risk. According to a CDC review, adults with arthritis were 2.5 times more likely to report two or more falls or experience a fall-related injury compared to adults without arthritis.1 Along with health care providers, program providers can help to increase awareness about the connection between arthritis and falls by promoting and implementing evidence-based programs for arthritis and fall prevention.
Resources to support the continuum
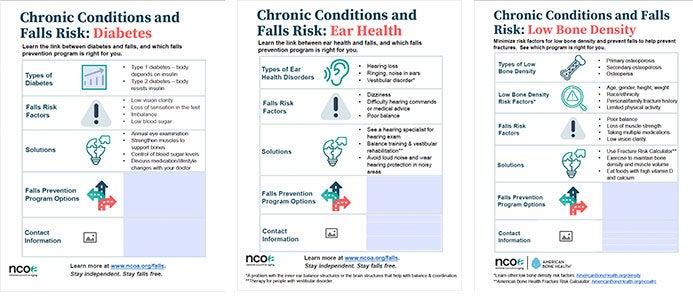
NCOA developed template flyers to help promote a continuum of programming. These flyers can help to educate participants on the benefits of falls prevention programs based on a particular chronic condition by highlighting the type of chronic condition, the related falls risk factors, solutions, and falls prevention program options. Organizations can add contact and logo information at the bottom of the flyer to connect community members to local program options.
- Chronic Conditions and Falls Risk: Arthritis
- Chronic Conditions and Falls Risk: Concussions
- Chronic Conditions and Falls Risk: Depression
- Chronic Conditions and Falls Risk: Diabetes
- Chronic Conditions and Falls Risk: Ear Health
- Chronic Conditions and Falls Risk: Heart Disease
- Chronic Conditions and Falls Risk: HIV
- Chronic Conditions and Falls Risk: Low Bone Density
- Chronic Conditions and Falls Risk: Multiple Sclerosis (People Who Use Wheelchairs and Scooters)
- Chronic Conditions and Falls Risk: Multiple Sclerosis (People Can Walk)
- Chronic Conditions and Falls Risk: Obesity
- Chronic Conditions and Falls Risk: Parkinson's
Depending on how participants are first connected to evidence-based programs in a community, they could enter the continuum in a variety of ways. Perhaps they first start with the Chronic Pain Self-Management Program or Chronic Disease Self-Management Program to learn skills and to build their confidence for managing their arthritis. They could then benefit from participating in Walk With Ease to safely increase their physical activity levels. Depending on their level of fall risk and/or their fear of falling, they could be a great candidate for either A Matter of Balance or Tai Chi for Arthritis and Fall Prevention. Or perhaps Tai Chi for Arthritis and Fall Prevention is their first workshop experience and through this, they learn about the Chronic Pain Self-Management Program to provide additional support in managing their arthritis.
Promoting physical activity guidance from the CDC could also be helpful. Ensure that participants understand that physical activity plays an important role in helping to manage chronic conditions, such as arthritis, heart disease and diabetes.2
If a participant in the Diabetes Self-Management Program (DSMP) has some vision loss and/or loss of feeling in the feet due to neuropathy, this can increase fall risk. As a result, perhaps they have limited their activity and have become more fearful of falling. In addition to the skills learned in DSMP, this person might benefit from participating in A Matter of Balance to learn cognitive restructuring skills and home safety tips to reduce the fear of falling.
Tips for engaging participants and partner organizations:
- Partner with local health care providers to host information sessions exploring the relationship between chronic conditions and fall risk. For example, host a fall risk screening at a diabetes workshop and refer participants to the appropriate fall prevention program or Diabetes Self-Management Program.
- Promote the continuum of programs that your organization offers with local health care providers.
- Meet with community providers to explore which programs are currently offered, and which programs could be added to support offering a continuum of programming; develop partnerships that could support offering this continuum.
- Evaluate your current program offerings. Do you have a broad range of programs that support the management of chronic conditions and fall risk? If not, review evidence-based programs that might complement your current offerings.
For additional resources and references on the links between chronic conditions and fall risk, please visit the continuum of programming resource on healthyagingnc.com.
This information is not meant as medical advice or diagnosis, nor is it meant to be a comprehensive overview of all chronic disease types, fall risk factors, solutions, or options. It is meant to encourage taking these into consideration when recommending programs.
Sources:
1. Barbour KE, et al. Falls and fall injuries among adults with arthritis—United States, 2012. Morb Mortal Wkly Rep. 2014;63(17):379-383. Found on the internet at https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6317a3.htm
2. Centers for Disease Control and Prevention. Physical Activity Programs. Found on the internet at https://www.cdc.gov/arthritis/interventions/physical-activity.html
This project was supported, in part by grant number 90CSSG0048 and 90FPSG0051 from the U.S. Administration for Community Living, Department of Health and Human Services, Washington, D.C. 20201. Grantees undertaking projects under government sponsorship are encouraged to express freely their findings and conclusions. Points of view or opinions do not, therefore, necessarily represent official Administration for Community Living policy.


