Eating Disorders Don’t Discriminate on the Basis of Age or Gender
8 min read

Liz remembers when she finally got up the courage to talk with her primary care physician (PCP) about the fact that she had been severely restricting her food intake. She had just reached the age at which her mother died, which sparked thoughts of all of the amazing things her mom had missed having left the world far too early. She didn’t want to miss out on her own children’s weddings and (hopefully) the birth of her grandchildren.
For Liz, it was easy to slip into an eating disorder as she aged
After reading an article on the impact of calorie restriction for longevity, Liz decided to give it a go. What she failed to realize was that prolonged caloric restriction for some people, perhaps those who are genetically predisposed, can be the first step into the quicksand that is anorexia nervosa. She rapidly lost 20 pounds and seemed to lose the ability to eat, even if she wanted to. She looked into the mirror and still saw herself as large, as if her self-image hadn’t kept up with her shrinking body.
Liz made an appointment with her PCP, who immediately noted her loss of weight. She said quite plainly, “Doc, I think I might have anorexia nervosa.”
He actually chortled, rolled his eyes, and responded, “Don’t be silly. Only young girls get anorexia nervosa. We need to work you up to see what is really going on.”
Liz felt humiliated and lost, and was unsure where to turn after her doctor failed to hear her concerns, blinded by his stereotyped (and inaccurate!) preconceptions of who develops anorexia nervosa.
Liz's story happens often and many older adults overlook signs of anorexia nervosa
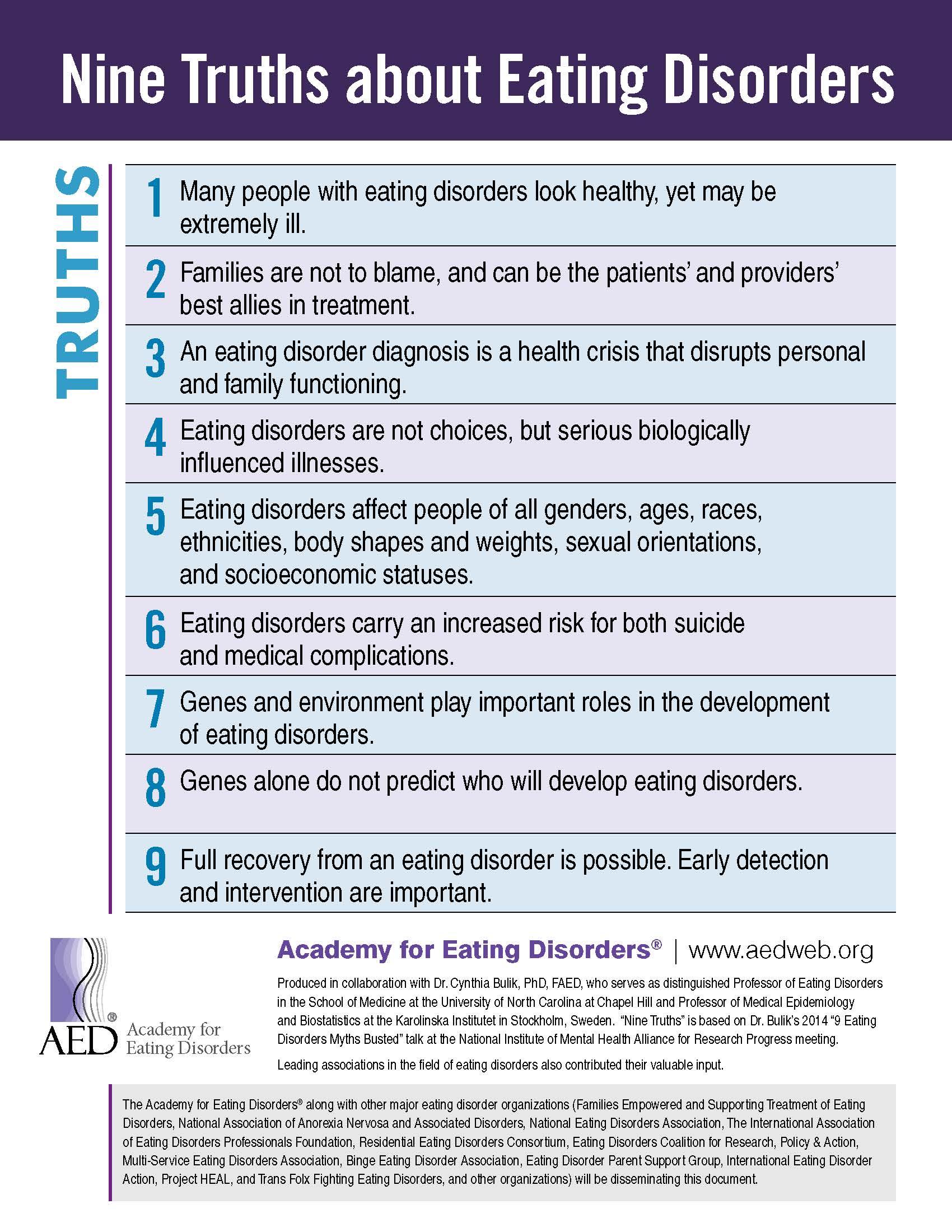
This same story is retold countless times by individuals whose profile falls outside of the stereotype of “young, white, affluent girls” who were the first to be recognized with anorexia nervosa. To counter the unhelpful stereotype, the Academy for Eating Disorders has published a valuable infographic called “The Nine Truths About Eating Disorders” (see image below) that was based on a lecture I gave at the National Institute of Mental Health in 2013.
If only Liz knew about the 'nine truths about eating disorders'
The Nine Truths have been translated into nearly 30 languages to spread facts about eating disorders around the world. Truth #5 states “Eating disorders affect people of all genders, ages, races, ethnicities, body shapes and weights, sexual orientations, and socioeconomic statuses.” In short, eating disorders don’t discriminate.
What are the different types of eating disorders?
The major eating disorders cover four basic presentations, but variations on the theme are the norm rather than the exception.
- Anorexia nervosa is marked by low body weight, a failure to recognize the seriousness of the illness, and undue influence on body weight and shape as determinants of self-esteem. Some people with anorexia nervosa maintain their low weight just by restricting their food intake. Others may also engage in driven physical activity to burn calories.
- Bulimia nervosa can occur at any body weight and is marked by binge eating (eating an unusually large amount of food in a short period of time together with a feeling that your eating is out of control) coupled with what are called “inappropriate compensatory behaviors” such as self-induced vomiting, laxative abuse, or other methods to undo the effects of a binge.
- Binge-eating disorder (BED) also includes binge eating, but in the absence of compensatory behaviors. People with BED can fall into the normal weight or higher weight ranges.
- in ARFID (avoidant/restrictive food intake disorder) people also restrict their food intake severely, but it does not include the psychological factors seen in anorexia nervosa such as drive for thinness. ARFID is much more than picky eating and it can take three overlapping forms: (1) sensory sensitivity (i.e., rejection of food based on sensory qualities such as texture); (2) phobic avoidance of food (i.e., concern about aversive consequences of eating such as fear of choking); and (3) low interest/appetite. We know much less about ARFID in mid-life and beyond as it is a fairly new addition to the catalog of eating disorders.
Who gets eating disorders in midlife?
Over the past decade, clinics around the world have been reporting an increase in women and men seeking treatment for eating disorders in midlife and beyond.
We see three general patterns. The most common pattern is people who may have had an eating disorder earlier in their life, and perhaps recovered fully or partially, and then their eating disorders rears its head again later in life, usually in response to some stressor, like in the case of Liz when she reached the age that her mother was when she died.
The second pattern is people who have had a long-standing eating disorder since earlier in their life and managed to survive, but are still suffering. It is important to know that eating disorders have the highest mortality rate of all mental illnesses, with the exception of the recent surge in overdose deaths from opiates.
The third pattern is those who develop eating disorders for the first time later in life. All three occur, and all three should be on the radar screens of all health professionals who work with older adults.
What causes eating disorders?
It is important to emphasize that eating disorders are caused by both genetic and environmental factors. Our research over the past few decades has shown a clear genetic component to the illness, and we are identifying specific regions of the genome that are associated with risk for these illnesses.
As stated in the Nine Truths, genes don’t act alone. Environment also plays a role. In fact, things in the environment can trigger an underlying genetic predisposition. Although an oversimplification of a complex process, genes load the gun, and environment pulls the trigger.
Eating disorders are not a choice, they are serious, genetically influenced mental illnesses.
What are the midlife triggers for eating disorders?
We see a range of triggers for mid- and late-life eating disorders, with many being associated with losses or transitions. Commonly reported triggers include children leaving home (or coming back after having left), loss of a partner, pressures of caretaking for older parents and children simultaneously, the impact of age discrimination, and concerns about ageing.
In terms of environmental triggers, the cosmetics industry also sows seeds of discontent among the older population by selling lotions, potions, and procedures that allege to make you look (and feel) younger. Their marketing of youth makes older people feel as if they can stop or at least slow down the train of aging. Marketers make us unhappy with our looks and encourage behaviors such as dieting, excessive exercise, and cosmetic surgeries that can be those first steps toward developing an eating disorder.
What are the medical consequences of eating disorders in midlife and beyond?
Eating disorders at any age take a terrible toll on every bodily system. The consequences differ somewhat depending on which eating disorder is experienced. Systems affected include musculoskeletal (osteoporosis), gastrointestinal, cardiovascular, dermatological, reproductive, and even dental. The complicating factor about eating disorders in midlife and beyond is that these systems all become more vulnerable as we age. Eating disorders take an even greater toll on an aging body than on a young one.
How can someone with an eating disorder find help?
Just like Liz’s story, it may not be straightforward to find help for eating disorders in midlife. Yet treatment is possible and typically involves a treatment team (physician, psychologist/therapist, dietitian). It is important to rule out other medical causes for weight loss or weight gain, especially in mid- and later life, but primary eating disorders should be considered as legitimate diagnoses in an older population. Currently there are no medications that are effective or approved for the treatment of anorexia nervosa or ARFID. Inpatient renourishment, residential treatment, and intensive outpatient therapy and nutritional counseling are cornerstones of treatment for these disorders. For bulimia nervosa and BED, the treatment of choice is cognitive-behavioral therapy. Each disorder has one U.S. Food and Drug Adminsitration (FDA) approved medication—fluoxetine [Prozac] for bulimia and lisdexamfetamine [Vyvanse] for BED)—although alone these medications do not lead to long-term cure and are best paired with psychotherapy to develop skills in managing eating disorder thoughts and feelings.
Support and understanding from partners and families also helps during the recovery process. We have created a couple-based intervention (Uniting Couples in the Treatment of Eating Disorders—UNITE) to help patients and partners recover from eating disorders as a team. The ultimate goal is to find health care professionals who are open to understanding and treating eating disorders in later life and to work closely with them to develop a recovery plan. Recovery from eating disorders can and does occur at any age.
A few resources for more information on midlife eating disorders
Books
- Midlife Eating Disorders: Your Journey to Recovery by Cynthia Bulik, PhD
- Pursuing Perfection: Eating Disorders, Body Myths, and Women at Midlife and Beyond by Margo Maine, PhD
Websites
- National Eating Disorder Association
- National Alliance for Eating Disorders
- Eating Disorder Hope
- Academy of Nutrition and Dietetics
NCOA hosts the annual Older Adult Mental Health Awareness Day to highlight critical issues in addressing mental health needs as we age.
This article is supported by the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $5 million with 100% funding by ACL/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by ACL/HHS, or the U.S. Government.