How 79-Year-Old Mary Turned Her Osteoporosis Diagnosis Into a Falls-Prevention Strategy
6 min read
Related Topics
“You can drink all the milk you want, but it’s not going to make a difference!”
That’s what Mary Welsh, 79, learned the hard way in the decades since she first was diagnosed with osteopenia.
Back then, conventional wisdom suggested that dietary calcium—highly present in milk and other dairy products—was the best protection against age-associated bone loss. And that wisdom wasn’t entirely wrong.
“There’s no doubt or disagreement among the medical community that consuming a calcium-rich diet, especially when we’re young, is crucial for strong, healthy bones,” explained Dorothea Vafiadis, Director of NCOA’s Center for Healthy Aging. “We have a limited period of time to achieve what’s called ‘peak bone mass’—generally between early adolescence and age 30 for most people—and that’s when dietary calcium packs its most powerful punch.”1
Because calcium helps build bone, it stands to reason that it helps maintain it, too. But it’s on this point that conventional wisdom begins to … fracture. In fact, as early as 1989—right around the time Mary’s doctor discovered her bone loss—researchers were questioning the role of calcium for preventing osteoporosis.
“Population studies generally have not demonstrated a strong relationship between calcium intake and bone loss,” one study concluded.2 Many others followed.
“The take-home message,” Vafiadis said, “is that starting out with the strongest bones possible absolutely helps later in life, because every single one of us begins to experience bone thinning as we age.
“Calcium can slow that process down, and that’s important,” she continued.
But once we’re past peak bone mass, eating high-calcium foods or taking supplements won’t help build new bone or necessarily protect against breaking one.”
Calcium, as Mary now knows, can’t reverse osteopenia once it starts. Nor will it cure osteoporosis.
Mary’s osteoporosis story
Mary was in her early 50s and recently past menopause when her gynecologist suggested a newfangled test.
“He had just gotten this machine—it looked like a fax machine or a photocopier—that supposedly measured the bone density of your wrist,” Mary recalled. “He wanted to use me as a guinea pig.”
Mary readily agreed. At the very least, she figured her status as an active adult with a healthy diet would provide a normal baseline.
She figured wrong.
The machine—a precursor to today’s DXA scanner—showed that she already had experienced some bone loss.
Because Mary had a healthy lifestyle, “we both were surprised by my results,” she said. That’s when she realized what Vafiadis earlier explained. Diet matters when it comes to osteoporosis. But other risk factors contribute, too.
Mary’s osteoporosis risk factors
As a post-menopausal woman, Mary already fell into the typical profile for the condition when she agreed to that wrist scan. She also checked a few more boxes, including having a low body weight and a small frame.
“On top of that, I was a heavy smoker when I was younger and was completely unaware that it was affecting my bone health,” she said. “I was destroying my bones, even though I ate a lot of spinach!”
Other risk factors that Mary did not have include:
- Sedentary lifestyle
- Calcium and Vitamin D deficiencies
- Low body weight and a small frame (body mass index less than 18.5 kg/m2)
- Certain chronic conditions, such as diabetes
- Certain medications, such as steroids
- Consuming more than two alcoholic drinks per day for men or one alcoholic drink per day for women3
“Family history matters, too,” Vafiadis explained, “but many of today’s older adults don’t have that information about their mothers, grandmothers, or aunts because physicians didn’t know to ask.”
That’s why Mary advises that any older adult concerned about their bone health ask their doctor about getting screened. “Even men,” she said. (After attending an educational session at her local senior center in Baltimore, Maryland, Mary learned that men aren't immune to osteoporosis.)
She has some other advice, too, which revolves around her biggest fear: falling and breaking a bone.
Mary’s osteoporosis rules for avoiding falls
Prescription drugs have dramatically slowed Mary’s bone loss since she was first diagnosed. And because osteoporosis medication also improves bone density, Mary’s bone strength likely has improved, too (increased bone density leads to greater bone strength).
“That’s good,” she explained, “because I have osteoporosis in my spine, which is really scary.”
According to Mary, osteoporosis hasn’t changed her life all that much. Still, it did spark a healthy fear of falling that guides her to this day. Mary knows that one in four older adults in the U.S. is likely to fall in any given year. She also knows that when older adults with osteoporosis fall, they are more likely to break a bone4—a potentially catastrophic event.
These so-called “fragility fractures” often happen in low-impact situations that wouldn’t normally result in a break in someone with normal bone density. But people with low bone density can easily fracture a hip, a wrist, or an arm simply by falling down from a standing position.5 Spine fractures can be even more insidious. They happen silently, often without a fall, and progress slowly over time.
“These fractures can compromise a person’s ability to walk, cause deformities and loss of height, and dramatically lower their quality of life,” Vafiadis said. “Osteoporosis may even indirectly lead to death, since fractures and related complications can cause an older person’s health to quickly deteriorate.”
That’s why Mary takes some very specific steps to avoid falls. She might even call them rules.
How to avoid falls when you have osteoporosis
- Staying active. Regular exercise, especially the weight-bearing kind, keeps muscles strong—and strong muscles protect bones and promote good balance. Mary walks most days of the week and takes a fitness class at the senior center.
- Eliminating tripping hazards. Furniture, area rugs, and even pets can cause falls in the home. Mary looked around her house and moved—or removed—any obstacles that posed a danger.
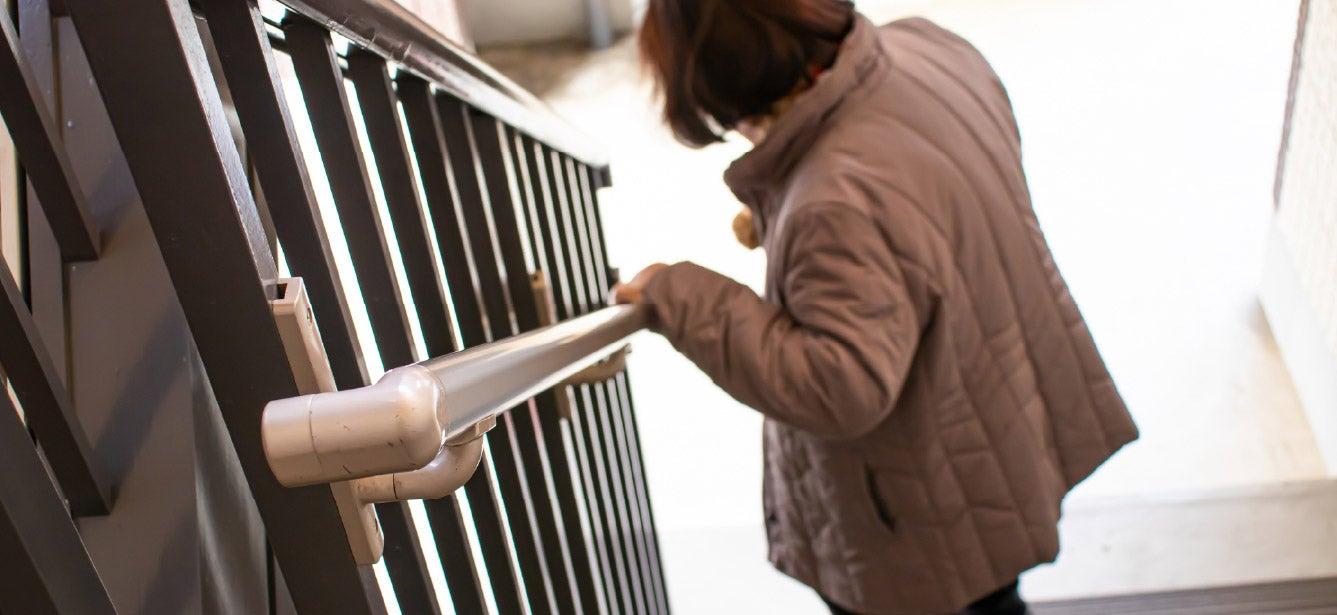
- Being aware of surroundings. Tripping hazards exist nearly everywhere, yet staying home to avoid all danger can create a vicious cycle of further physical decline and an increased risk for falls. Mary constantly scans the sidewalk for cracks, uneven surfaces, and even wet leaves during her walks. She also makes sure always to use the railings when climbing or descending stairs.
- Asking for help. Standing on a chair to dust the top of a tall cabinet or reach a hard-to-get holiday decoration may seem like a good idea—but the margin of error is small. When the urge hits, Mary reminds herself not to do it and leans on family instead.
“I try to obey my own rules,” she said with a laugh. She even has toned down activities she used to engage in without much thought, like swimming in the surf and swinging her small grandchildren into the air.
“I know both of those things could knock me down, so I stay on the sidelines now,” she concluded. Doing so helps ensure that Mary can continue to experience the greatest joy in her life: spending time with her family, preferably at the beach.
Mary’s story, and our content covering bone health for older adults, was developed in partnership with Amgen. Learn more about Amgen’s commitment to supporting the osteoporosis community through innovative research, treatments, and education.
Sources
1. JAmerican Academy of Orthopaedic Surgeons. OrthoInfo. Healthy Bones at Every Age. Found on the internet at https://orthoinfo.aaos.org/en/staying-healthy/healthy-bones-at-every-age/
2. .A. Kanis, et al. Calcium supplementation of the diet—II. British Medical Journal, 28 January 1989. Found on the internet at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1835554/
3. Academy of Nutrition and Dietetics. Osteoporosis. Found on the internet at https://www.nutritioncaremanual.org/topic.cfm?ncm_toc_id=272432
4. National Osteoporosis Foundation. Osteoporosis Fast Facts. Found on the internet at https://www.bonehealthandosteoporosis.org/wp-content/uploads/2015/12/Osteoporosis-Fast-Facts.pdf
5. International Osteoporosis Foundation. Fragility Fractures. Found on the internet at https://www.osteoporosis.foundation/health-professionals/fragility-fractures




