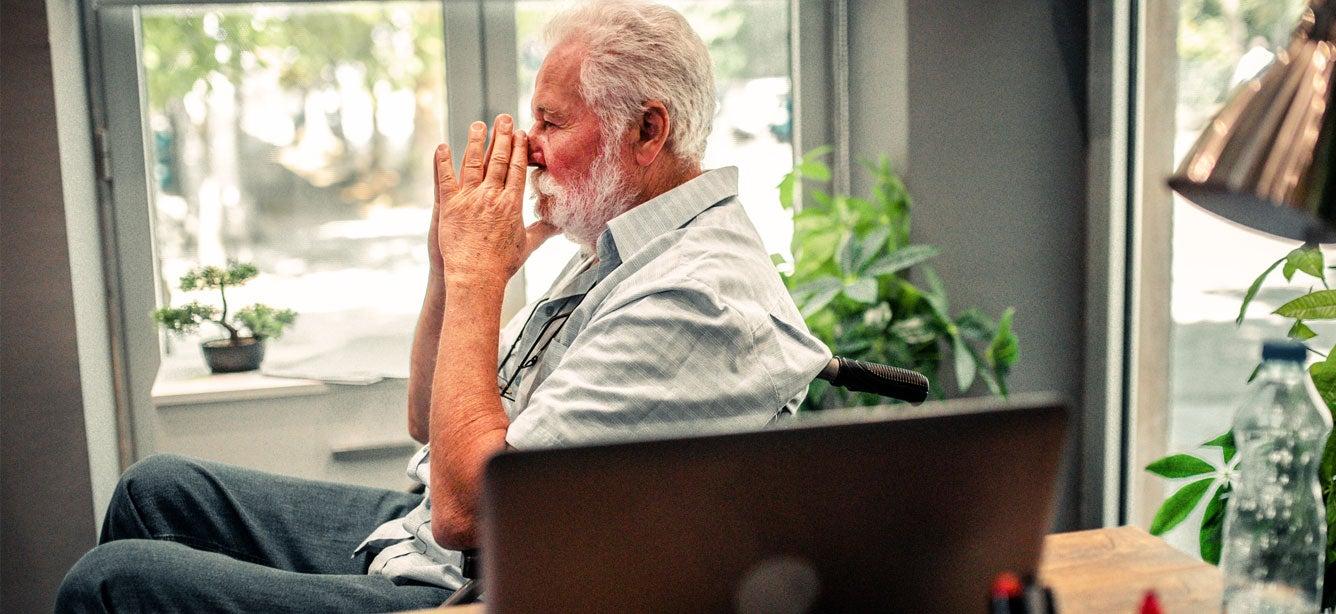
Behavioral Health
Older adults are less likely to access mental health treatment, whether due to stigma, lack of access to providers, or the misconception that conditions like depression, anxiety, or others are a normal part of aging. Learn more about how to support your community.

Getting the Care You Need via Telemedicine
Oct 23, 2025

Get the Facts on Healthy Aging
May 09, 2025
What Is Substance Abuse?
Jan 24, 2025
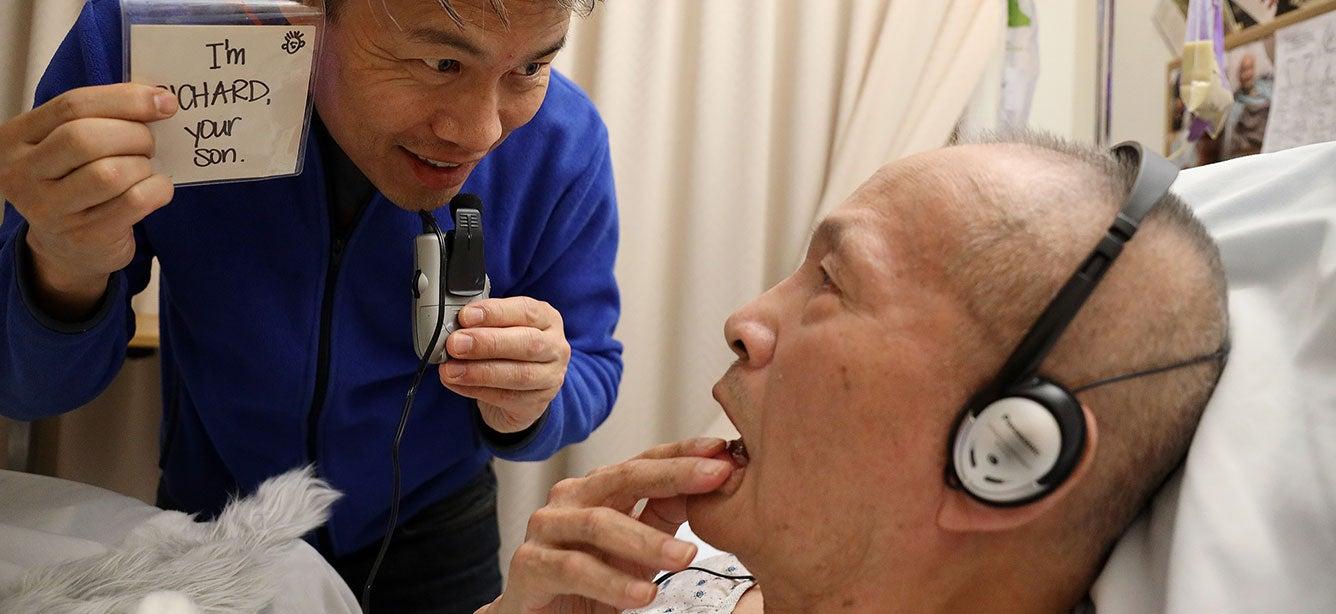
Help from the 988 Lifeline
There are caring people who want to help you, no matter what problems you’re dealing with. If you or an older adult you care about is struggling, dial or text 988 now to speak with a Lifeline counselor.