How to Successfully Involve Community Health Workers in Delivering Evidence-Based Programming
8 min read
More and more organizations are employing or working with community health workers (CHWs) to better help their communities and address health-related social needs. The National Association of Community Health Workers defines CHWs’ role as “champions" who are "striving to build a healthier community.”
CHWs, who can go by other titles such as Promotores de Salud, outreach worker, community advocate, or health navigator, to name a few examples, are the trusted members of the community they serve. They are community educators, capacity-builders, advocates, and liaisons for underserved communities.
CHWs address the needs of individuals facing barriers to health care access. They are the frontline workforce and serve as the link that brings individuals in the community to health and social services. Because of such diverse roles throughout the country, the CHW Core Consensus Project has worked to define and establish a national consensus to increase “the visibility and greater understanding of the full potential of CHWs.”
Community health workers make great evidence-based program leaders
Given CHW’s well-established quality in their connection to the community they serve and their comprehensive skill set, they can make an excellent fit to lead or refer to evidence-based programs (EBP). While CHW certification programs vary from state to state, many CHWs are equipped with core knowledge in topics like chronic conditions, mental health, and community resources.
CHWs are also trained to have skills that would match well to serve as an EBP leader such as communication, interpersonal and relationship building, education and facilitation, outreach, engagement, and advocacy.
CHW initiatives at Rush University Medical Center
NCOA visited the Rush University Medical Center (CDSME 2022 and Fall Prevention 2023 grantee) in Chicago in late 2023. During the visit, RUSH’s commitment and actions to improve the quality of life within their neighboring communities was evident. As one of the leading organizations to integrate social care into clinical care, RUSH prioritizes addressing the cause of poor health—social, economic, and environmental factors—and promoting prevention and management of chronic conditions and risk factors to improve the quality of life in their communities, while providing medical care.

In 2018, RUSH launched the Community Health Worker Hub. The Hub's mission is "to respond to community needs as they arise through resource connection, health promotion and education, and advocacy with a CHW workforce that represents the communities we are serving." During the COVID-19 Pandemic, the importance and effectiveness of CHWs in connecting people in their community to RUSH's medical care and to other resources became evident. Since then, the Hub has grown to have approximately 30 full-time CHWs and Lead CHWs.
"There are no CHWs without our social workers, either," says Robyn Golden, Associate Vice President of Social Work and Community Health and Chair of the Department of Social Work at RUSH. Working closely and collaboratively with RUSH's licensed social workers and registered nurses, the team of these professionals and experts has become an essential component of RUSH's efforts.
From the beginning, RUSH has strategically hired individuals as CHWs from the neighborhood as RUSH saw the importance of ensuring their staff are representatives from the communities they serve. The CHW team is currently comprised of 21 women and eight men. They are passionate about and committed to their community’s well-being. Their unique skill set has been a must to meet the needs of its communities more efficiently and effectively in West Side Chicago, where the average life expectancy is as low as 66-69 years in some neighborhoods and as high as 82 in another according to the RUSH’s Community Health Needs Assessment conducted in 2022.1

As RUSH prioritizes disease prevention as a tool to improve life expectancy in its neighborhood, many of RUSH’s CHWs are certified to lead evidence-based health promotion programs such as Chronic Disease Self-Management Education (CDSME) Programs and Falls Prevention Programs. Because of their well-established relationship with their community, and with their skills to engage people into important conversation, these workshops led by CHWs have been significantly successful.
How CHWs build stronger, inspired, heathier communities
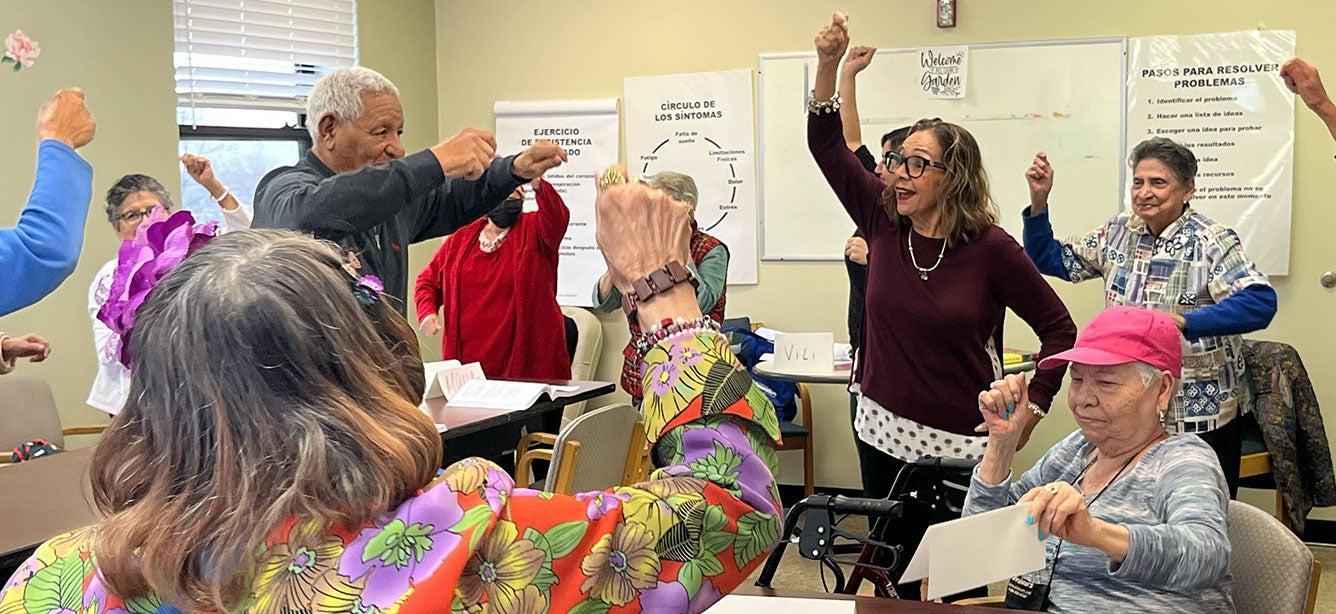
Even when the relationship is new, a close and strong bond with implementation partners seems to quickly form through CHWs. During the site visit, we had an opportunity to visit and meet the director and staff from the Circle Resource Center (The Circle), a resource center for women in Brightonpark, IL with the RUSH’s Office of Social Work and Community Health team. Yessenia Cervantes-Vazquez, one of the Lead CHWs and a Master Trainer of CDSME programs, facilitates Tomando Control de su Salud, a Spanish version of the Chronic Disease Self-Management Program (CDSMP) there. The moment we walked into the center, the director and staff warmly welcomed us in. “Yessenia is like a daughter to me. We are family. Everyone loves learning from her”, said the director. Yessenia and the director had known each other for less than a year since the Circle was introduced as a potential CDSMP implementation partner. “I always wondered what this beautiful building was for whenever I drive by here to go to the school right behind it. Now this place feels like home,” said Yessenia.
The Circle and Yessenia together hosted four Tomando Control de Salud workshops with full classes of 14 to 15 participants at a 100% retention rate. The participants are fully engaged, sharing their experiences and learning together. Some of the participants and the staff also became interested in becoming leaders, building the capacity to implement the programs collaboratively. RUSH also plans to offer other CDSME and Falls Prevention programs in the coming months.
Another example of this heartwarming story we heard was from Ebony, another Lead CHW. She taught a CDSME workshop, and then several months later, she was at a nail salon in her neighborhood where she ran into two of the former workshop participants. Of course, they recognized each other and went on to informally check in on their action plans. The participants shared that they had kept exercising, and actually walked to the salon.
Ensuring CHW professional development and career growth
Treating individual CHWs as professionals, full-time employees, and as team members is also emphasized at RUSH. This focus has paved the way for RUSH’s CHWs to be formally involved as professionals in community health through a medical institution and build their careers. As a result, RUSH has a strong team of committed and dedicated members.
While leading evidence-based programs are a central part of the CHW roles, they also play crucial roles including:
- Providing resources at health fairs, shelters and Rush@Home visits
- Promote the CDSME and Fall Prevention programs
- Connecting individuals to care through appointment navigation and benefits enrollment
- Identify needs for REACH students (youth program)
To support these multiple roles, RUSH ensures to provide support and paths for professional development within the organization. CHWs at RUSH receive not only the core training but also additional training to enhance their skills. For example, Mental Health First Aid was recently added to the training to support CHWs as they often encounter difficult situations with their clients. CHWs are given autonomy to determine how to best reach the communities. There are opportunities for monthly case consultation to debrief and brainstorm about community health needs and resources. This approach seems to be different from what they have seen elsewhere with other CHWs they encounter.
CHWs are also trained to utilize the closed-loop referral platform to track referrals and create a personalized document of resources after completing SDOH screenings. Their workflow is embedded in the hospital referral system to ensure each older adult continues to receive necessary resources through Rush’s vast network in the community after the first encounter.
Braiding funding for sustainability
As with many of the public health related initiatives, securing and maintaining a funding stream is one of the biggest challenges for organizations that rely on CHWs. At RUSH, the CHWs and their services are funded through public dollars, grants, private individual donors, philanthropic dollars, and federal funding.
While there seems to be always plenty of support for the CHW initiative at RUSH, it has not been the case. Management has constantly advocated for the importance and effectiveness of CHWs internally and externally to maintain and grow its capacity and infrastructure. Collecting tangible data, documenting case studies and testimonials, and sharing them have been the most powerful tools to prove and get buy-ins from other stakeholders and funders.
Recognizing the evidence in value of CHW’s interventions and services in addressing health disparities in medically underserved communities, many states have begun taking various strategies to support and sustain the CHW workforce through state and federal funding source. These sources including Medicaid reimbursement for CHW delivered evidence-based programming as part of Medicaid State Plan Amendments, 1115 demonstration waivers, and Managed Care Organization approaches.
Interested in learning more about how other communities are engaging CHWs in Evidence-Based Programs? Watch this four session webinar series to learn about CHW initiatives by the Administration for Community Living (ACL) Chronic Disease Self-Management Education and Falls Prevention Program grantees in Minnesota, New Mexico, and South Dakota.
Sources
1. Rush University Medical Center. Community Health Needs Assessment (CHNA) and Community Health Implementation Plan (CHIP) Reports. CHNA/CHIP Reports and CBR. Found on the internet at https://www.rush.edu/about-us/rush-community/chnachip-reports-and-cbr
This project was supported, in part by grant number 90CSSG0048 and 90FPSG0051 from the U.S. Administration for Community Living, Department of Health and Human Services, Washington, D.C. 20201. Grantees undertaking projects under government sponsorship are encouraged to express freely their findings and conclusions. Points of view or opinions do not, therefore, necessarily represent official Administration for Community Living policy.



