How can you find out about the quality of a Medicare health care plan before you buy it? That’s where Medicare Star Ratings come in. Whether you're enrolling in Medicare for the first time or looking to switch plans, these ratings provide a clear, simple way to understand how different plans measure up.
What are the Medicare star ratings?
The Star Ratings system was developed by the Centers for Medicare & Medicaid Services (CMS). It rates Medicare Advantage (Part C) and prescription drug (Part D) plans on a 5-star scale with 1 being the lowest score and 5 being the highest score.
| ⭐⭐⭐⭐⭐ | Excellent |
| ⭐⭐⭐⭐ | Above average |
| ⭐⭐⭐ | Average |
| ⭐⭐ | Below Average |
| ⭐ | Poor |
Ratings focus on health plan quality based on measurements of customer satisfaction and the quality of care a plan delivers.
The goal of Star Ratings is to improve the quality of care and general health status for people with Medicare. This rating system also supports the efforts of CMS to improve the level of accountability for the care provided by physicians, hospitals, and other providers.
How do I find a Medicare plan's Star Rating?
You can find the Star Ratings for current Medicare Advantage or Part D plans by using the Medicare Plan Finder tool. Five-star plans will have a special star icon beside them. CMS reviews and updates Star Ratings annually. The final ratings are released in October of each year. If plans are new to the marketplace, they will not have ratings.
Medicare Advantage plans are given an overall rating based on five unique categories:
- Member experience with the health plan: This is measured by members' personal reviews of a plan.
- Customer service: This is based on how well the plan responds to and handles member complaints and appeals.
- Plan performance: This focuses on member complaints and changes in the plan’s performance. It includes how often Medicare found problems with the plan, how often members had problems with the plan, and how much the plan's performance has improved over time, if at all.
- Chronic conditions: This is based on how often members with certain long-term conditions were recommended tests and treatments to help manage their condition.
- Staying healthy: This category measures whether members received various screening tests, vaccines, and preventive check-ups to help them stay healthy.
Medicare Part D (prescription drug) plans are given an overall rating based on four categories:
- Member experience with the drug plan: This is based on members' personal reviews of the Part D plan.
- Customer service: This measurement is based on how well the plan manages member complaints and claim appeals.
- Plan performance: This focuses on member complaints and changes in the plan’s performance. It includes how often Medicare found problems with the plan, how often people had problems with the plan, and how much the plan's performance has improved (if at all) over time.
- Drug safety and pricing: This category measures how accurate the plan’s pricing information is, and how often people with certain medical conditions are prescribed drugs in a way that is safer and clinically recommended for their condition.
Why are Medicare Star Ratings important?
Star ratings provide additional points of comparison, along with costs and coverage, when you’re shopping around for a Medicare plan. A 5-star rating is considered excellent. A Medicare plan with less than 3 stars is considered poor quality and not likely to provide the best health care options.
What is the 5-star Special Enrollment Period?
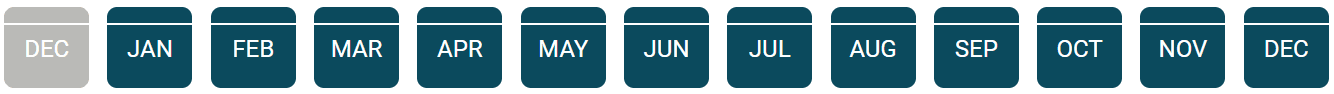
If there’s a 5-star Medicare Advantage plan or Part D drug plan available in your area, you can use what’s called the 5-Star Special Enrollment Period to switch from your current Medicare plan to a Medicare plan with an excellent quality rating. You can take advantage of this opportunity only once between Dec. 8 (after the Open Enrollment Period) and Nov. 30 of the following year.
Other periods in which you can enroll in a Star-Rated Medicare Advantage or Part D plan include:
- Initial Enrollment Period: This period is for people who are new to Medicare. It takes place during the three months before, the month of, and the three months after your 65th birthday.
- Open Enrollment Period: This takes place Oct. 15–Dec. 7 annually, for those already enrolled in Medicare and who want to switch plans.
- Special Enrollment Period: These are opportunities older adults have outside of the Initial and Open Enrollment Periods to change Medicare Advantage plans, if they meet certain conditions.
When is my Special Enrollment Period?

What is the Special Enrollment Period for Disenrollment?
If you're enrolled in a lesser-rated Medicare Advantage or Part D plan, are you stuck with it? Luckily, the answer is no. The Special Enrollment Period for Disenrollment from lower-rated plans is available once per calendar year between Jan. 1 and Dec. 31. If you’re enrolled in a plan that has received a Star Rating of fewer than 3 stars for three straight years, you can use this time to switch to a plan rated 3 stars or better. You can also switch to a newer Medicare plan that has not yet been rated.
Keep in mind: For both of these Special Enrollment Periods, you may lose your Part D coverage if you move from a Medicare Advantage plan that has drug coverage to a 5-star Medicare Advantage Plan that does not have this coverage. You may have to wait until the next Open Enrollment Period to get drug coverage, and you may end up with a late enrollment penalty. The Part D late enrollment penalty is a monthly add-on premium calculated as 1% of the current national base beneficiary premium multiplied by the number of uncovered months, rounded to the nearest 10 cents.
Who can help me choose the right Medicare plan?
If you’re wondering, “How do I get unbiased Medicare advice?”, a great place to start is contacting your local State Health Insurance Assistance Program (SHIP).
SHIPs offer unbiased Medicare counseling provided by trained staff members and volunteers. Your SHIP counselor can walk you through your options for Medicare coverage and help you identify the plan(s) that best fits your needs. They can also help you apply for benefits that can save you money on your Medicare costs, such as Medicare Part D Extra Help or the Medicare Savings Programs (MSPs).